A groundbreaking algorithm from UCLA is rewriting the rules of diagnosis, offering hope for underrepresented communities and finding cases that human doctors miss.
- Radical Improvement in Detection: UCLA’s new AI tool identifies approximately 80% of undiagnosed Alzheimer’s cases, nearly doubling the accuracy of previous models.
- Bridging the Racial Divide: The algorithm specifically targets disparities in healthcare, ensuring equitable diagnostic accuracy for Black, Latino, and East Asian populations who are often overlooked.
- The Power of Early Action: By catching the disease years earlier, the tool opens the door for new therapies and crucial lifestyle changes, potentially slowing the disease’s progression.
Alzheimer’s disease currently stands as the sixth leading cause of death in the United States, casting a long shadow over millions of families. Despite its prevalence, the medical community faces a startling hurdle: studies indicate that up to 40% of Alzheimer’s cases remain undiagnosed until the disease has significantly progressed. To combat this “invisible” crisis, researchers at UCLA are harnessing the sophisticated power of artificial intelligence to identify at-risk patients long before traditional methods would catch them.
The Science of Seeing the Unseen
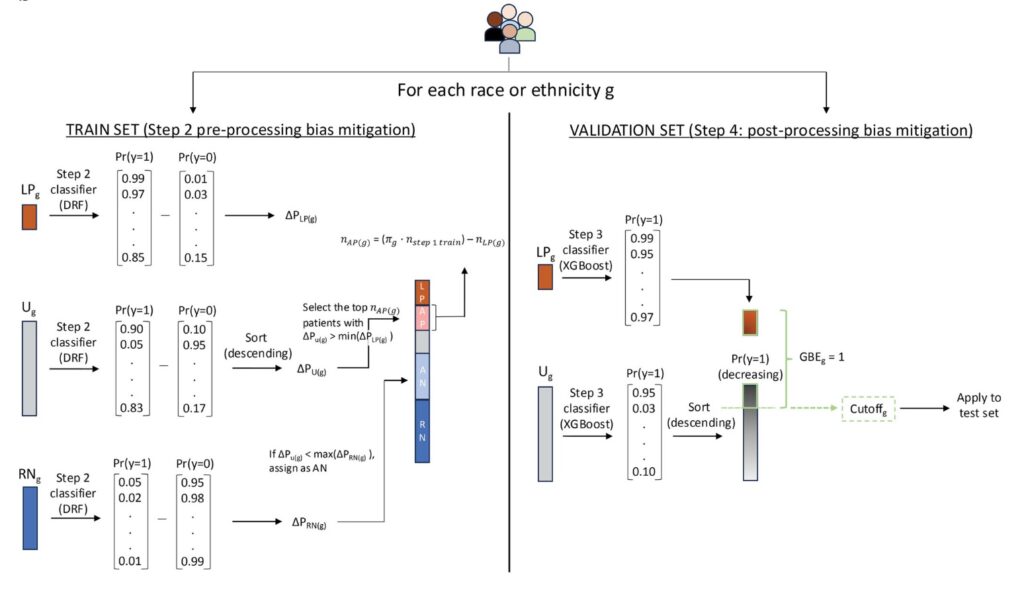
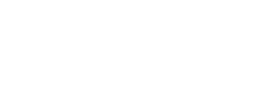
The core of this breakthrough lies in a specific type of machine learning known as “semi-supervised positive unlabeled learning” (SSPUL). Unlike standard models that only learn from confirmed cases, this algorithm dives deep into electronic health records to analyze a complex web of data, including prior diagnoses, age, and various neurological indicators.
According to Dr. Timothy Chang, a UCLA neurologist involved in the research, the results have been transformative. “We were able to capture about 80% of the people who actually would have undiagnosed Alzheimer’s disease,” Chang explained.
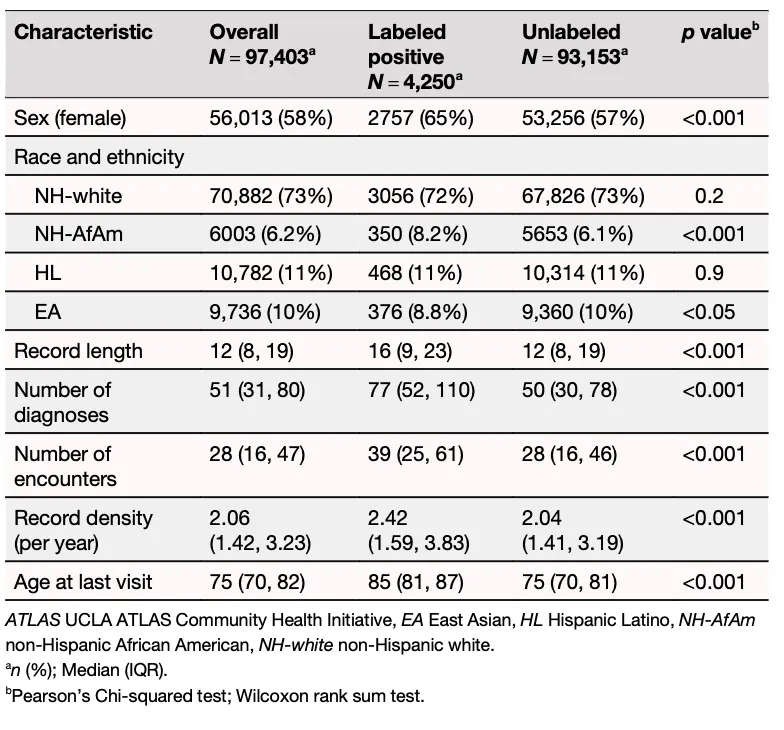
The statistical data backs up this claim. While standard supervised baseline models struggled with a sensitivity rate of only 0.39–0.53, the UCLA team’s SSPUL method achieved a superior sensitivity of 0.77–0.81. This massive leap in accuracy means the tool is nearly twice as effective at flagging potential cases, identifying both neurological markers, such as memory loss, and less obvious non-neurological signals, such as decubitus ulcers.
Eliminating Bias in Medicine
One of the most critical aspects of this new tool is its focus on equity. Historically, Black people and Latinos are statistically more likely to develop Alzheimer’s but are significantly less likely to receive a timely diagnosis compared to other groups.
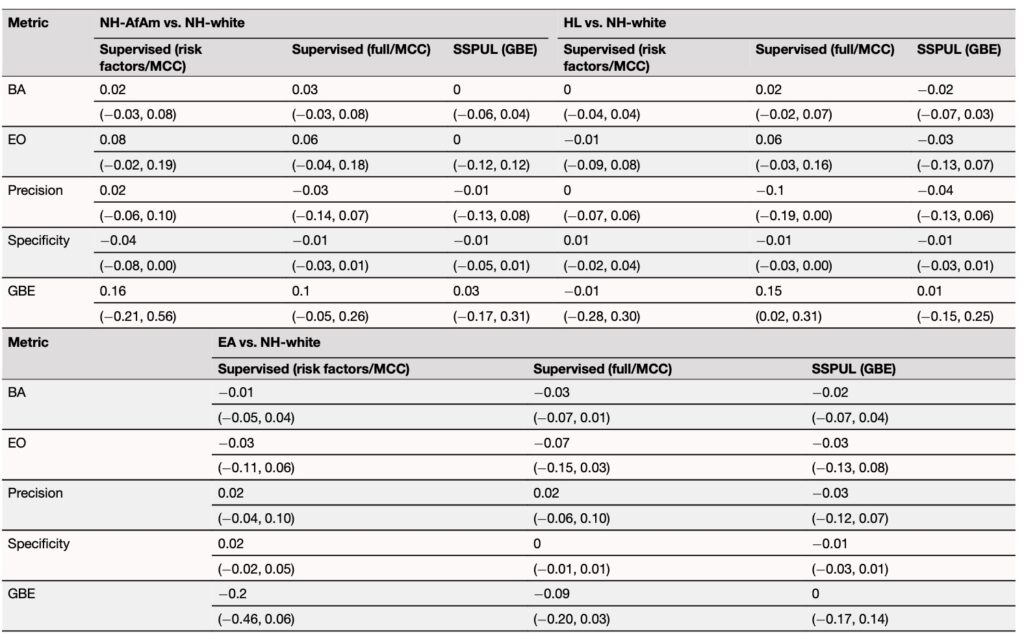
To address this, the researchers engineered the AI with racial bias mitigation at its forefront. They performed rigorous “sensitivity analyses,” which involved recoding race and ethnicity data within the system to ensure the model wasn’t making predictions based on bias. For example, researchers tested if the model’s prediction changed when a patient’s race was recoded from Non-Hispanic White to Non-Hispanic African American while keeping all other medical features fixed.
The result was a model that exhibited superior fairness with the lowest “cumulative parity loss.” The AI maintained its high precision (Area Under the Precision Recall Curve of 0.81–0.87) across Non-Hispanic White, African American, Hispanic Latino, and East Asian groups. “It does it fairly across different groups,” said Dr. Chang, noting that the tool helps level the playing field for underrepresented patients.
Validation Through Data
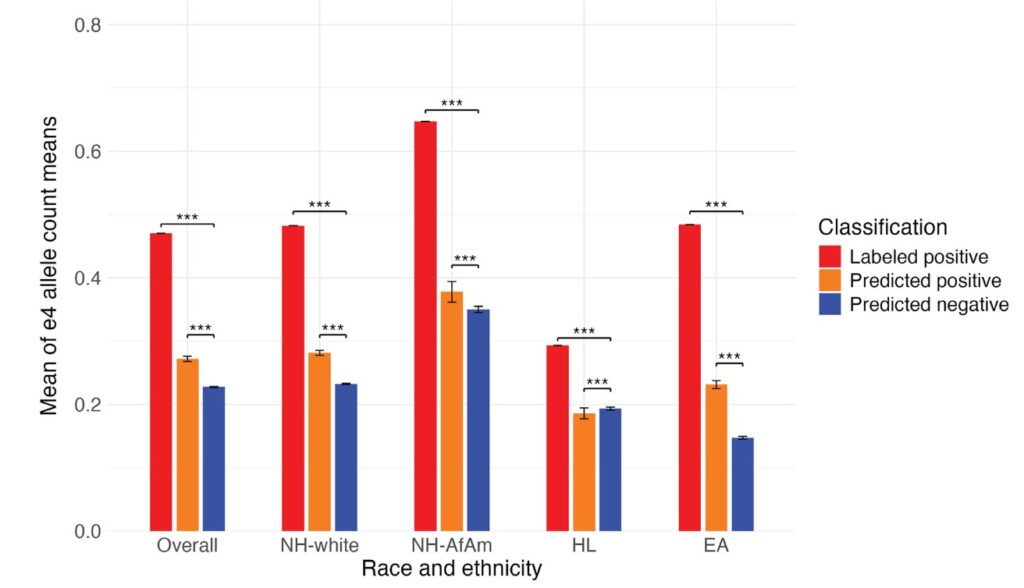
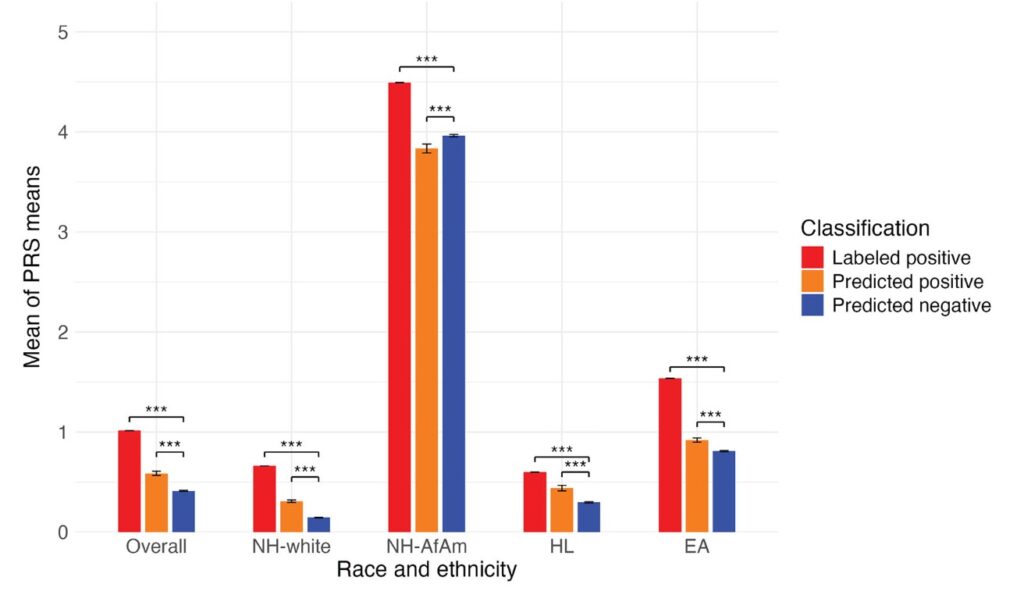
The researchers did not stop at training the model; they subjected it to intense validation stress tests. They utilized polygenic risk scores—genetic indicators of disease risk—to verify the AI’s findings. The results showed that risk scores were significantly higher (p<0.001) in patients the AI predicted were positive for Alzheimer’s compared to those it flagged as negative, confirming the biological accuracy of the computer’s predictions.
Furthermore, the team tested the model’s robustness against “proxy label distribution shifts.” By removing specific diagnostic codes and medications from the data sets and re-running the algorithms, they ensured the AI wasn’t just “cheating” by looking for obvious keywords but was actually identifying the underlying pathology of the patients.
The Human Cost of Late Diagnosis
Behind the complex algorithms and statistical values are real families struggling with the realities of dementia. Ana Kelly, whose mother Anita Chavira passed away in 2016 due to Alzheimer’s, knows the pain of late diagnosis all too well.
“I had come to realize that she did have dementia years before she was actually diagnosed,” Kelly recalled. By the time the diagnosis came, her mother’s health had already begun a steep decline.
Kelly’s experience, which was featured in a USC student documentary, has shaped her view on the importance of the early detection this AI tool provides. With a shortage of caregivers looming for the growing number of Americans facing dementia, Kelly believes knowledge is power. “If I should ever get it, I would like to be a cooperative patient and family member,” she said. “I don’t want to make it more difficult for my loved ones to take care of me.”
A Window for Intervention
The ultimate goal of this AI tool is not just to diagnose, but to buy time. Dr. Chang emphasizes that early identification allows patients to access new therapies that are only effective in the early stages of the disease. Furthermore, it empowers individuals to make lifestyle changes—improving eating habits, increasing exercise, and prioritizing mental health—that can alter the disease’s trajectory.
As Kelly poignantly noted, “If I can’t prevent it, I can at least slow it by a decade or two. That would be important to me.” Thanks to the intersection of advanced artificial intelligence and medical science, that extra decade is becoming a reachable possibility for millions.